Two weeks ago, the Employees Provident Fund (EPF) published “Belanjawanku” (My Budget), an expenditure guide for individuals and
families living in the Klang Valley. It has generated some debate amongst the
Malaysian public, with most doubtful of the fact that it is possible for a
single youth to rent a room for only RM300 in the area. There was, however, no
real public discourse on the RM30 budgeted for healthcare. Leaving aside those
who have either purchased private health insurance or have health issues,
respondents must be feeling very healthy and optimistic, and consequently
likely did not think of allocating much of a health budget. RM30 would not be
sufficient to secure any private
insurance plan.
Granted, treatment for minor illnesses would likely be affordable
under such a budget. This isn’t the case for more serious ailments, however.
The 2019
Global Medical Trend Rates Report
published by Aon, an international professional services consultant firm, forecasts net growth of 13.6% in Malaysia’s medical
inflation rates for current year – almost 5.7 times the forecast for inflation
in general (Figure 1). The 2017
Malaysia National Health Expenditure
findings also indicate that expenditure on medical goods already comprised 8%,
or RM4.55 billion, of total health expenditure. This is a conservative
calculation, one which does not include similar expenditures for inpatients.
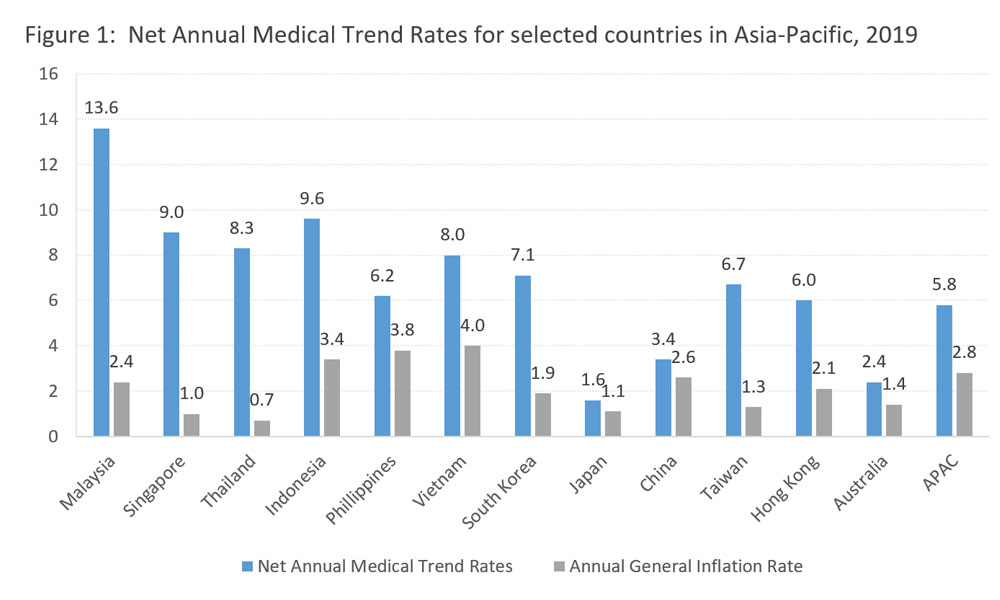
Source: “2019 Global
Medical Trend Rates Report”, Aon
The
federal government in 2017 provided approximately RM2.4 billion for the
procurement of medical drugs. This took up 10% of the total MOH budget in 2017.
This expenditure item saw an increase of 13% relative to the preceding year,
but medical supply shortages remain a problem in some public clinics and
government hospitals - especially during the end of the year. This implies that
the demand for public medical supplies still exceeds supply.
Unlike
ordinary commodities, such as soft drinks where consumers are spoilt with
choices and could have always opt out from purchasing such products, the
purchase of medicine is entirely different. Under normal circumstances,
patients are left with no choice but to seek treatment, particularly if their
illness demands immediate attention. There are no alternative products to very specific
drugs, especially when originator drugs are still under the patent protection
period. This further limits the choices of patient seeking alternative medicine.
What really makes the difference is the phenomenon of asymmetric information
within medicine, where the judgments and drug prescription decisions of doctors
and pharmacists dictate or limit the choices a patient faces.
Some
are led to believe that originator drugs must be more superior than generics in
terms of quality, efficacy and safety, and are therefore willing to pay a much
higher price for the originator even if they were told about the existence of
its generic counterpart. In Malaysia, after the successful registration of a
drug patent, a product will usually enjoy a period of 20 years of market
exclusivity. When the originator drug is still under intellectual property
protection, it may be the market’s only option for a particular disease, and
this is when the price a drug can fetch is usually at its peak. Originator drug
manufacturers normally consider the cost of drug production – including
investment in R&D – and operating costs (including marketing),
stakeholders’ interests, as well as consumers’ purchasing power and their
willingness to buy the drug in a particular country, before they set the final
price tag for their product.
The
reality is that generic drugs have the same active pharmaceutical ingredient,
dosage, administration route and functional effectiveness as originator drugs.
It is only when the patent for the originator drug has expired that generic
drugs are approved to be sold in the market. The production cost and sale price
of generic drug is generally significantly lower than that of the originator, even
if the latter would later adjust their price to compete with the generic
alternative.
According
to the Medicine
Prices Monitoring 2017 report, the final retail
prices for generics are on average 3 times cheaper than originators.
Consequently, price-sensitive consumers typically choose generics. In 2017, the
average availability of generics in the public sector was 74.8% compared to
originators (19.4%) (Figure 2). This is in line with the national medicine
policy which encourages the use of generic medicines. However, the private sector
has a tendency to use originators more often, with an average availability of
52.2%.
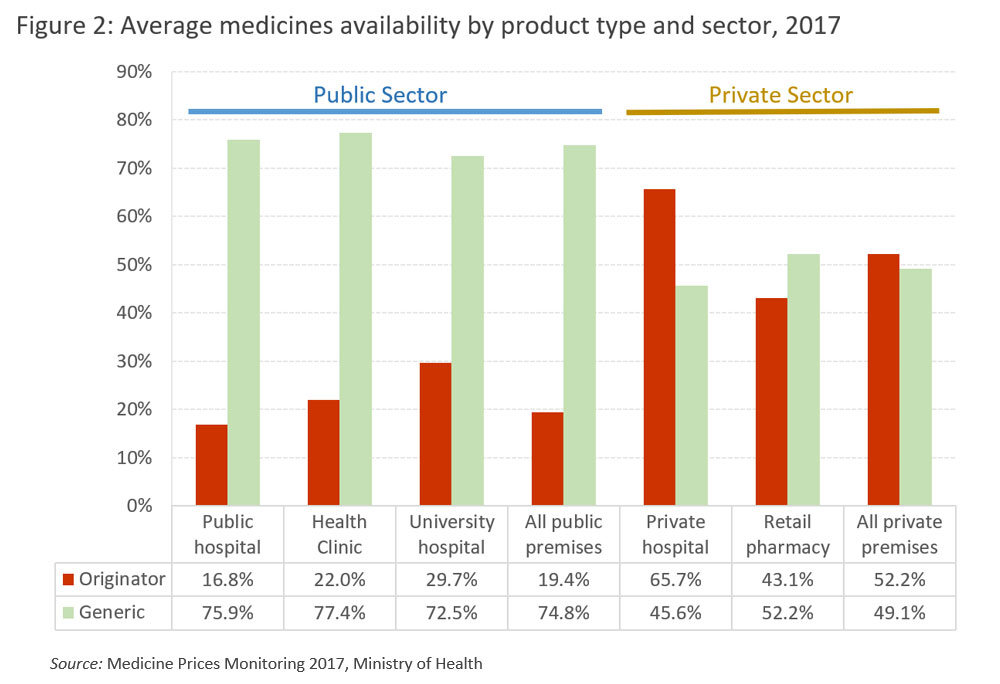
Source:
Medicine Prices Monitoring 2017, Ministry of Health
In neighbouring Philippines, the law stipulates that the doctors and pharmacists must provide at least two generics (if they do exist) to accompany a prescription of an originator drug. This approach expands the availability of drug choices for patients.
In a normal medicine supply chain, drugs are produced by the manufacturer, ordered and shipped by importers, before changing hands to wholesalers or distributors who are in charge of the delivery of the products to the retailers (hospitals, clinics and pharmacies). Finally, they will reach the hands of patients or consumers. Due to the many levels of transactions within the supply chain, drug prices are inadvertently marked up at every level. Public healthcare system eschews the final retail-level mark-up, as our public healthcare system is tasked with providing medicine to the needy at almost zero cost.
Malaysia has a pharmaceutical manufacturing sector which produces almost entirely generic drugs, with sales revenue amounting to only a quarter of the total revenue of the pharmaceutical industry in 2014-2015. Some 61 percent of drugs (of equivalent revenue value) are imported, and amongst those, 87 percent of revenues were in the hands of local proxy companies for the big multinational pharmaceutical manufacturing companies. The top five companies take 47 percent of total medicinal imports, and importantly, these big multinational pharmaceutical parent companies get to decide the drug prices across countries, and they normally sell originator drugs.
Although local importers and sales proxies representing the top five multinational pharmaceutical companies did not have a big net profit margin (in between 1.6 and 3.4 percent), the average net profit margin for their parental companies is 26.2 percent - about 10 times that of their local importers! This market phenomenon indicates that the drug price-setting practice and global sales has laid golden eggs for Big Pharma companies, and left a bitter taste for patients and governments who have to make these purchases. Critics often point out that the market behaviour of the pharmaceutical companies has a significant impact on global medical inflation.
Distributors
only work for the clients, provide logistics, and storage and services support,
but do not own any stock of medicine. This is so they would not have influence
over market pricing. A
market review report shows that the mark up by
wholesalers or distributors was marginal, at 2-3%. However, when the products
reached the retailers – such as medical institutions and pharmacies – the
mark-up is different.
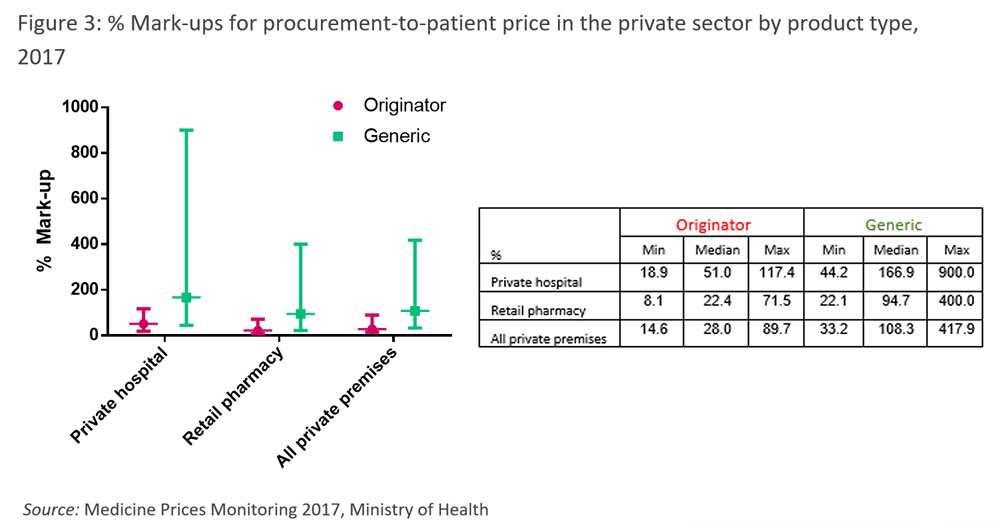
According
to the Medicine Prices Monitoring 2017 report, the median mark-up for
originators’ and lowest-priced generics’ retail price in private hospitals was
51% and 167%, respectively, whereas in pharmacies these figures were lower, at
22.4% and 94.7% (Figure 3). This shows that the mark-up range can be exceedingly
large; in some extreme cases, in private hospitals these could even spike up to
117.4% and 900%! Due to the lower production or import cost of generic drugs,
this in turn allows private hospitals, clinics and pharmacies the opportunity
to further mark up the final retail price which results in higher prices across
the board, but greater profits.
Those
in the sector often claim that price setting operations for medical products
are within the bounds of the free market, or in other words, that mark-up
behaviour is totally within legal boundaries, although it is considered by many
to be unethical. Particularly when the prices for prescription or controlled
medicines are hardly transparent, it is difficult for consumers to clearly
compare prices and make informed decisions. In fact, the free market dogma
entails that prices be made transparent so that market could be made more
efficient, with consumers making the best decision for themselves!
However,
the situation we have now often ‘encourages’ retailers to raise their prices
arbitrarily while patients or consumers are not properly informed. Patients
receiving medical treatment services often find that medicinal purchases
constitute the most significant expenditure item in medical bills; this
indicates that the mark-ups set by medical institutions undeniably add to
patients’ financial burdens.
Two
months ago, I participated a conference on rising medical costs. Throughout the
conference, representatives from the participating multinational pharmaceutical
companies, local private hospitals, as well as chain pharmacies all claimed
that their profits are entirely justifiable because margins are reasonably low.
A representative of a local chain pharmacy even commented to the audience that
the large volume of medical products they sold were only of such a small profit
to them that they have to diversify and rely on selling ice cream to subsist!
This claim blatantly contradicts what data indicates.
Dealing
with the factors contributing to rising drug cost, the Ministry of Health (MOH)
has mooted the introduction of a mechanism to control
medicine prices. This would be an interesting,
if complex and challenging, proposal. Besides this, the pharmaceutical services
department under the MOH is making efforts to increasing the transparency of
medicine prices. Therefore, since 2015 a Consumer Price Guide
has been uploaded on their website to enable people to make price comparisons.
In the name of fairness and transparency, I hope the private sector takes the
initiative to display all retail medicine prices to allow the public to make
informed judgments. After all, for a laissez-faire
market to work efficiently and effectively, there should be a free flow of
pricing information for consumers to make the most economical decisions.
The article was published here at Malaysiakini, Opinion, March 17, 2019